Abstract
Background: Many genetic drivers that are implicated in disease pathology and risk stratification have been identified for pediatric acute myeloid leukemia (pedi-AML). However, only a minority have been exploited for therapeutic interventions and most of the identified genetic events currently lack targeted therapy to address the mutations. The combined consequences of genetic and epigenetic events culminate in a net effect manifested at the protein level and most of the chemotherapies target proteins. Yet little is known about the proteomic landscape of pedi-AML.
Methods: Reverse Phase Protein Array (RPPA) was performed with 291 strictly validated antibodies to determine the protein expression levels of bulk leukemic cells from 505 pedi-AML patient samples that were collected prior to therapy. All patients participated on the COG AAML1031 Phase 3 clinical trial, that compared standard therapy (ADE) to ADE plus bortezomib (ADE+B). Proteins were allocated into 31 protein functional groups (PFG) (e.g. cell cycle, apoptosis) to analyze proteins in relation to related proteins. Progeny clustering was performed to identify patients with correlated protein expression patterns within each PFG (protein cluster). Block clustering searched for protein clusters that recurrently co-occurred (protein constellation), and for subgroups of patients that expressed similar combinations of protein constellations (protein signatures). Protein signatures were correlated with known cytogenetics and mutational state.
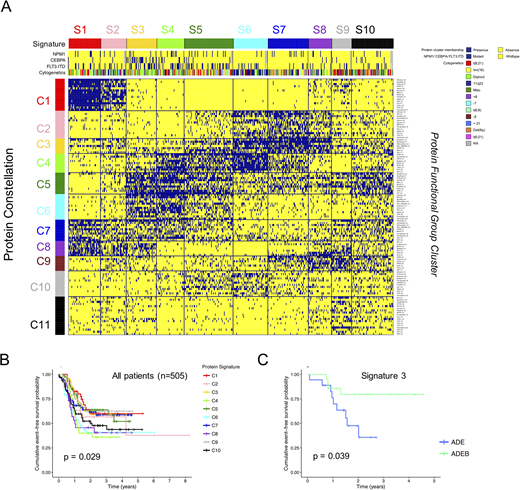
Results: For each PFG, cluster analysis identified an optimal number of protein clusters, resulting in a total of 120. From this we constructed 11 protein constellations (PRCON) and 10 protein signatures (SIG) (Fig. 1A). A training set (n=334) and test set (n=171) showed high reproducibility (Pearson's X2; p < 0.001). SIG were prognostic for event-free survival (EFS) (p = 0.029), with a favorable EFS for SIG 1, 2, 3, 5, 7 & 9, and an unfavorable EFS for SIG 4, 6, 8, 10. Notably, patients that formed SIG 3 had a significant better EFS after receiving ADE+B than patients that received ADE (p = 0.039) (Fig. 1B). This SIG was highly enriched for CEBPA mutated cases; 43% vs. 9% overall (p < 0.001). SIG were associated with cytogenetic aberrations (p < 0.001) and mutational state, as well as with the traditional risk groups (p < 0.001). For example, t(8;21) was overrepresented in SIG 9 (39% vs. 16% overall) and MLL-rearrangement in SIG 6 (61% vs. 19% overall). Multivariate analysis was performed using variables definable at time of diagnosis and known prognostic factors. This resulted in a final model including unfavorable protein SIG together with low risk cytogenetics and NPM1 mutation state as independent prognostic factors, suggesting that proteins add to known prognostic factors.
Proteomics could also identify aberrantly expressed proteins within each SIG compared to normal CD34+ cells. This recognized 31 proteins as universally down regulated (e.g. CDKN1A, PPP2R2A) and 13 as universally up regulated (e.g. PIK3CA, NCL). Many other proteins were different between SIG, and thus potentially targetable in particular patient groups: high KIT (SIG 3, 4 & 5), high BCL2 (SIG 3, 4, 5, 6, 9 & 10) and high BRD4 (SIG 6). SIG 1 & 2 both had a very characteristic expression pattern and were most distinct from the others. IGFR1, IGFR1.pY1135, AKT3, SMAD5.pS463-7 and RICTOR.pT1135 were all high, whereas they were low in most other SIG. Conversely, STAT3 was normal in SIG 1&2, but changed in the other SIG. SIG 6, 7 & 8 also had relatively similar expression patterns, but had different outcomes. Compared to SIG 6 & 8, SIG 7 had higher GAB2 and MCL1 and lower RAD50, ERCC1.
Conclusions: Pedi-AML is characterized by a finite number (n=10) of recurrent protein signatures. SIG were only partially correlated with cytogenetics and mutation state, indicating that protein expression could add to genetics in the process of risk stratification. We identified SIG that did well vs. SIG that did not, independent of known risk factors, and identified a group of patients that could potentially benefit from ADE+B. Recognition of differentially expressed proteins suggest potential targets for combinational treatment (Hoff et al. ASH HSF1 abstract).
Figure 1. A. Identification of 11 PRCON (horizontally) and 10 SIG (vertically). B. SIG were prognostic for EFS. C. SIG 3 significantly benefitted from ADE+B (green) compared to ADE alone (blue).
Kolb:Roche- Genentech: Membership on an entity's Board of Directors or advisory committees; Servier: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal